Kyphosis
Kyphosis: Symptoms, Diagnosis and Treatment
Kyphosis Meaning:
Kyphosis means an abnormal forward bending of spine leading to round back/ hunchback deformity. Spine has natural curves when seen from the side: cervical and lumbar lordosis, and thoracic kyphosis. Lordosis is convexity to the front and kyphosis is concavity to the front. In kyphosis, either thoracic kyphosis is exaggerated or there is loss of normal lordosis.
Types of Kyphosis:
- Scheuermann’s Kyphosis: Also called Developmental Kyphosis, this is counterpart of Idiopathic Scoliosis as real cause behind development of deformity is not known. Anterior part of vertebral bodies (especially in Thoracic Spine) grows at a slower rate than posterior. This usually causes a rigid deformity. Patients have back pain along with a cosmetic deformity. Boys are affected more commonly. Usual age of presentation is 12-15 years. Patient may have difficulty in sleeping on back due to the abnormal curvature
- Congenital Kyphosis: Some patients have bony abnormality within the vertebrae. There may me abnormal union or absence of anterior part of the vertebral bodies. These curves are usually acute and progress rapidly. Congenital Scoliosis is usually associated with intra-spinal anomalies (Tethered Cord, Diastematomyelia), and various heart, kidney, abdominal disorders.
- Postural Kyphosis (Slouching): Postural kyphosis is usually flexible and corrects on lying down. This is mostly present in tall individuals and girls during puberty.
- Secondary Kyphosis: Kyphosis can also occur due to various disease processes destroying anterior part of vertebral column, e.g.
- spine infection/ spinal tuberculosis,
- spine fracture/ osteoporotic fractures,
- spinal tumors (Multiple Myeloma).
Symptoms of Kyphosis:
Primary symptom of kyphosis is cosmetic spine deformity. Congenital Kyphosis usually have acute curve, which is cosmetically more disfiguring. Many patients have associated back-pain. Patient may have breathing difficulty in severe cases due to compression of chest.
Spinal cord compression might happen with severe deformity, especially in Congenital and Secondary Kyphosis. This might lead to symptoms of spinal stenosis (loss of sensation and weakness in arms/ legs, loss of bladder-bowel control, loss of dexterity and weakness in hand grip, loss of balance and spasticity in legs).
Diagnosis of Kyphosis:
A thorough history and physical examination is required to assess magnitude of deformity and ascertain possible cause of scoliosis. A detailed neurological examination is must to rule out spinal cord involvement. Patient’s primary complaint need to be understood (concern about future worsening, cosmetic problem, difficulty in sitting-standing, back pain, neurological symptoms).
Following tests are required:
X-ray: X-ray is first and most important diagnostic tool. It will show magnitude of the curve. X-ray can be repeated at regular intervals to assess worsening of the curve for patients who are under observation. Anterior and posterior bending x-rays will reveal flexibility of the spine deformity and will help spine specialist choose correct surgical procedure. Osteoporotic vertebral fractures and bone destruction from trauma/ infection/ tumor will be revealed.
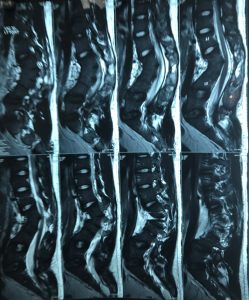
MRI Scan: MRI will also reveal spinal cord and bone anomalies in Congenital and Secondary Scoliosis. MRI will reveal cause and extent of the primary disease process in Secondary Kyphosis. MRI will show spinal stenosis and degenerative changes in degenerative cases. MRI should always be done before surgery is planned.
CT Scan: A CT is required whenever a detailed assessment of bone anatomy is required, as in Congenital Kyphosis and Spinal Fractures/ Spinal Infections. A 3D reconstruction of spinal model is very helpful in planning spine deformity surgery. CT will also help in choosing the best method of instrumentation.
EMG NCV: To assess abnormal nerve function.
Other Tests: USG abdomen and cardiac 2D Echo are required to rule out other congenital anomalies (Congenital Scoliosis). A biopsy might be required to rule out spinal tumors/ spinal infections is suspected cases.
Treatment of Kyphosis:
Best treatment for kyphosis varies from patient to patient and is based on age at presentation, type of kyphosis, severity of the curve etc. It can be divided in three broad categories:
- Observation: Patients are kept under observation if:
- Deformity is not severe requiring immediate bracing or surgery,
- Cosmetic disfigurement is not significant,
- There are no neurological problems,
- Treatment by bracing/ surgery is not possible (very young age, debilitated patients, associated medical problems etc.)
It is very important to keep a close eye on every patient presenting with spinal deformity for following reasons-
-
- A young patient has high chance of progression of spinal deformity due to remaining growth spurts and long period remaining for growth.
- Congenital and Secondary Scoliosis as they have high chances of progression,
- Case with high risk of developing neurological problems, e.g. congenital scoliosis, secondary scoliosis.
These patients require regular follow up every 3-4 months to assess worsening of deformity by clinical and x-ray examination. Patients with Postural Kyphosis are benefited significantly by physiotherapy and posture correction exercises. Physiotherapy will also help in reducing the backpain and improve muscle strength.
- Bracing: Brace is recommended for patients with Scheuermann’s Kyphosis when Cobb Angle is 60-80 degrees and child is growing. A full time (> 20 hours/ day) use of brace is required. The aim of bracing is to 1) prevent further progression of the curve to possibly avoid surgery, 2) To postpone the surgery. Bracing will not work for patient who have attained skeletal maturity. Bracing does not reverse the curve. A regular follow up with clinical examination and x-ray is essential during bracing period to check for progression of the spinal deformity requiring change in bracing or possible need of spine surgery. Brace might need to be changed several times during the treatment to adjust for growth of the body.
Brace is also used for patients with Secondary Scoliosis to provide support to the spine. This will provide pain relief and will prevent sudden vertebral collapse which can cause increased pain, worsening of deformity and spinal cord compression. Bracing is not useful for congenital and traumatic kyphosis.
- Surgery (Deformity correction, instrumentation and fusion): Surgical correction is best treatment for scoliosis in following situations:
- High magnitude Scheuermann’s Kyphosis (> 80 degrees),
- Curves showing progression despite bracing/ casting,
- Cosmetic disfigurement,
- Body imbalance,
- Curves with impending/ associated neurological symptoms.
- Congenital and Secondary Scoliosis as they have high likelihood of progression.
Primary aim of surgery in kyphosis is to prevent worsening of the curve and to get as much correction as possible safely. Various surgical techniques are available. Most commonly, a posterior approach is used. Spinal segments in the curve are aligned and fused with the help of instrumentation. It is aimed to keep instrumentation level to minimum as instrumented part of the spine will lose its movements causing spinal stiffness. In certain cases, an anterior surgery is required to loosen a rigid deformity to achieve better correction by posterior surgery.
An early surgery is advised in Congenital and Secondary Kyphosis as these curves progress rapidly and have high risk of causing neurological problems. These risks increase if curve is severe. Curves with higher magnitude are difficult to correct, are usually only partially correctable with unsatisfactory cosmetic results, and have high complication rate. An anterior surgery is more commonly required in these cases to release the spine for better correction, decompress the spinal cord from front and reconstruct the deformed/ destroyed vertebral bodies. This can be either done separately from a front approach or can be done simultaneously during posterior surgery.
Computer navigation and spinal neuromonitoring are very useful for severe kyphosis deformity correction.
Recovery after kyphosis surgery is fairly quick. Patients are allowed to sit and walk very next day after the surgery depending upon their pain tolerance. Advanced pain management protocols help minimize the pain during recovery.



Kyphosis, characterized by an excessive outward curvature of the upper back, is a condition that concerns many individuals. As a spine surgeon, I often encounter patients eager to know if kyphosis can be reversed. While the extent of reversal depends on various factors, including the severity and underlying causes, there is hope for improvement.
Conservative Approaches: In mild cases of kyphosis, conservative treatments like physical therapy, postural exercises, and ergonomic adjustments can help reduce symptoms and improve posture. These measures aim to strengthen the muscles supporting the spine and alleviate discomfort.
Surgical Intervention: In more severe cases, surgical intervention may be considered. Spinal fusion surgery can correct the curvature by realigning the vertebrae and stabilizing the spine. This surgical approach can significantly improve the curvature and relieve associated symptoms.
Early Detection Matters: The key to successful reversal lies in early detection and intervention. Regular check-ups and screenings, especially during adolescence when kyphosis can develop, are essential. Early diagnosis allows for timely management and can prevent further progression.
In conclusion, while complete reversal of kyphosis may not always be possible, significant improvements can be achieved through conservative methods and, in severe cases, surgical intervention. As a spine surgeon, I am committed to providing personalized care and guidance to individuals seeking relief from kyphosis-related challenges. If you suspect you have kyphosis, don’t hesitate to consult with a specialist to explore your treatment options.
In the intricate world of spinal health, three common conditions often come into focus: kyphosis, lordosis, and scoliosis. These conditions, while distinct in nature, all affect the spine’s curvature and can impact an individual’s overall well-being.
Kyphosis: Kyphosis is a spinal disorder characterized by an excessive outward curvature of the upper back. This causes a rounded or hunched appearance, commonly referred to as a “hunchback.” It can result from factors like poor posture, osteoporosis, or congenital issues. Kyphosis can lead to discomfort, limited mobility, and pain, making early diagnosis and treatment crucial.
Lordosis: Lordosis, on the other hand, is the opposite of kyphosis. It involves an exaggerated inward curvature of the lower back. This condition, also known as “swayback,” can result from various factors, including obesity, muscle imbalances, or structural abnormalities. Lordosis may cause lower back pain and postural problems, making proper treatment essential.
Scoliosis: Scoliosis is a lateral curvature of the spine, where the spine deviates to the left or right. It often develops during adolescence and can have genetic or unknown causes. Scoliosis can lead to uneven shoulders, hips, and a visible spinal curve. Early detection through screening is crucial to prevent further progression and to manage the condition effectively.
In conclusion, kyphosis, lordosis, and scoliosis are distinct spinal conditions that affect the spine’s curvature. Timely diagnosis and appropriate treatment are vital in managing these conditions, ensuring a better quality of life and spinal health. If you suspect you have any of these conditions, consult a healthcare professional for an accurate assessment and personalized treatment plan.